Our Specializations
Urology
Treatment
- Treatment for kidney stones varies, depending on the type of stone and the cause.
Large stones and those that cause symptoms
- Using sound waves to break up stones: extracorporeal shock wave lithotripsy (ESWL)
- Surgery to remove very large stones in the kidney
- A procedure called percutaneous nephrolithotomy involves surgically removing a kidney stone using small telescopes and instruments inserted through a small incision in your back
- To remove a smaller stone in your ureter or kidney, your doctor may pass ureteroscope to your ureter through the urinary passage and break the stone into pieces that will pass in your urine
- Parathyroid gland surgery
Small stones with minimal symptoms
- Drinking water
- Pain relievers
- Medical therapy: alpha blockers include tamsulosin
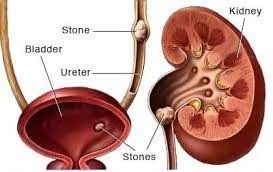
Kidney Stone
Kidney stones (also called renal calculi, nephrolithiasis or urolithiasis) are hard deposits made of minerals and salts that form inside your kidneys.
Passing kidney stones can be quite painful, but the stones usually cause no permanent damage if they’re recognized in a timely fashion.
Symptoms
A kidney stone usually will not cause symptoms until it moves around within your kidney or passes into your ureters — the tubes connecting the kidneys and the bladder. If it becomes lodged in the ureters, it may block the flow of urine and cause the kidney to swell and the ureter to spasm, which can be very painful. At that point, you may experience these signs and symptoms:
- Severe, sharp pain in the side and back, below the ribs
- Pain that radiates to the lower abdomen and groin
- Pain that comes in waves and fluctuates in intensity
- Pain or burning sensation while urinating
- Pink, red or brown urine
- Cloudy or foul-smelling urine
- A persistent need to urinate, urinating more often than usual or urinating in small amounts
- Nausea and vomiting
- Fever and chills if an infection is present
Causes
Dehydration: Inadequate fluid intake leads to concentrated urine, promoting the crystallization of minerals.
Dietary factors: High intake of oxalate-rich foods (spinach, nuts), sodium, and animal proteins can contribute to stone formation.
Genetics: A family history of kidney stones may increase susceptibility.
Medical conditions: Certain conditions, such as hyperparathyroidism and urinary tract infections, can enhance stone development.
Obesity: Higher body weight is associated with an increased risk of kidney stones.
Medications: Certain medications, including diuretics and antacids, may contribute to stone formation.
Underlying health issues: Digestive diseases and surgical procedures that affect nutrient absorption can lead to changes in urine composition.
Age and gender: Men are more prone to kidney stones, and the risk increases with age.
Geographical location: Some regions with high temperatures and low humidity may contribute to dehydration and stone formation.
Previous history: Individuals who have had kidney stones in the past are at a higher risk of recurrence.
RIsk Factors
- Family or personal history. If someone in your family has had kidney stones, you’re more likely to develop stones, too. If you’ve already had one or more kidney stones, you’re at increased risk of developing another
- Dehydration. Not drinking enough water each day can increase your risk of kidney stones. People who live in warm, dry climates and those who sweat a lot may be at higher risk than others
- Certain diets. Eating a diet that’s high in protein, sodium (salt) and sugar may increase your risk of some types of kidney stones. This is especially true with a high-sodium diet. Too much salt in your diet increases the amount of calcium your kidneys must filter and significantly increases your risk of kidney stones
- Obesity. High body mass index (BMI), large waist size and weight gain have been linked to an increased risk of kidney stones
- Digestive diseases and surgery. Gastric bypass surgery, inflammatory bowel disease or chronic diarrhea can cause changes in the digestive process that affect your absorption of calcium and water, increasing the amounts of stone-forming substances in your urine
- Other medical conditions such as renal tubular acidosis, cystinuria, hyperparathyroidism and repeated urinary tract infections also can increase your risk of kidney stones
- Certain supplements and medications, such as vitamin C, dietary supplements, laxatives (when used excessively), calcium-based antacids, and certain medications used to treat migraines or depression, can increase your risk of kidney stones
Prevention
- Drink water throughout the day
- Eat fewer oxalate-rich foods
- Choose a diet low in salt and animal protein
- Continue eating calcium-rich foods, but use caution with calcium supplements
Kidney stones (also called renal calculi, nephrolithiasis or urolithiasis) are hard deposits made of minerals and salts that form inside your kidneys.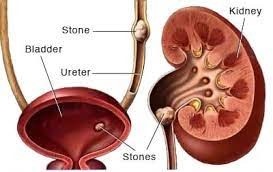
Passing kidney stones can be quite painful, but the stones usually cause no permanent damage if they’re recognized in a timely fashion.
Symptoms:
A kidney stone usually will not cause symptoms until it moves around within your kidney or passes into your ureters — the tubes connecting the kidneys and the bladder. If it becomes lodged in the ureters, it may block the flow of urine and cause the kidney to swell and the ureter to spasm, which can be very painful. At that point, you may experience these signs and symptoms:
- Severe, sharp pain in the side and back, below the ribs
- Pain that radiates to the lower abdomen and groin
- Pain that comes in waves and fluctuates in intensity
- Pain or burning sensation while urinating
- Pink, red or brown urine
- Cloudy or foul-smelling urine
- A persistent need to urinate, urinating more often than usual or urinating in small amounts
- Nausea and vomiting
- Fever and chills if an infection is present
Risk factors:
- Family or personal history. If someone in your family has had kidney stones, you’re more likely to develop stones, too. If you’ve already had one or more kidney stones, you’re at increased risk of developing another
- Dehydration. Not drinking enough water each day can increase your risk of kidney stones. People who live in warm, dry climates and those who sweat a lot may be at higher risk than others
- Certain diets. Eating a diet that’s high in protein, sodium (salt) and sugar may increase your risk of some types of kidney stones. This is especially true with a high-sodium diet. Too much salt in your diet increases the amount of calcium your kidneys must filter and significantly increases your risk of kidney stones
- Obesity. High body mass index (BMI), large waist size and weight gain have been linked to an increased risk of kidney stones
- Digestive diseases and surgery. Gastric bypass surgery, inflammatory bowel disease or chronic diarrhea can cause changes in the digestive process that affect your absorption of calcium and water, increasing the amounts of stone-forming substances in your urine
- Other medical conditions such as renal tubular acidosis, cystinuria, hyperparathyroidism and repeated urinary tract infections also can increase your risk of kidney stones
- Certain supplements and medications, such as vitamin C, dietary supplements, laxatives (when used excessively), calcium-based antacids, and certain medications used to treat migraines or depression, can increase your risk of kidney stones
Treatment:
Treatment for kidney stones varies, depending on the type of stone and the cause.
Small stones with minimal symptoms:
- Drinking water
- Pain relievers
- Medical therapy: alpha blockers include tamsulosin
Large stones and those that cause symptoms:
- Using sound waves to break up stones: extracorporeal shock wave lithotripsy (ESWL)
- Surgery to remove very large stones in the kidney
- A procedure called percutaneous nephrolithotomy involves surgically removing a kidney stone using small telescopes and instruments inserted through a small incision in your back
- To remove a smaller stone in your ureter or kidney, your doctor may pass ureteroscope to your ureter through the urinary passage and break the stone into pieces that will pass in your urine
- Parathyroid gland surgery
Prevention:
- Drink water throughout the day
- Eat fewer oxalate-rich foods
- Choose a diet low in salt and animal protein
- Continue eating calcium-rich foods, but use caution with calcium supplements
A blockage in the kidney’s renal pelvis (upper end of the ureter) is called a ureteropelvic junction (UPJ) obstruction. Blocking urine flow can damage the kidney.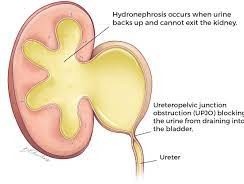
It is responsible for about 80% of all swollen urine-collecting systems. Males are affected at more than double the rate of females, and the left kidney is affected about twice as often as the right.
Symptoms:
- Lump in the abdomen
- Urinary tract infection with fever
- Pain in the upper abdomen or back, usually after drinking fluids. In some cases, pain may come and go because the blockage isn’t complete, allowing urine to flow at times. In other instances, blockage may occur only when the person is standing upright but not when lying down
- Kidney stones
- Blood in the urine
- Vomiting
- Poor growth in an infant
Causes:
Most UPJ obstructions are present at birth, an indication that structures of the ureter or kidney did not form correctly as the fetus was developing.
In some cases an inherited tendency to obstructions will run in a family, but usually an obstruction appears in just a single family member.
A number of different types of obstructions may be present at birth, such as:
- The opening of the ureter is too narrow
- There are mistakes in the number or arrangement of small-muscle cells in the ureter. These cells are responsible for the muscular contractions that push urine from the kidney down to the bladder
- Unusual folds in the walls of the ureter may act as valves
- Twists may form along the path of the ureter
- The ureter connects to the renal pelvis in too high a position, creating an abnormal angle between the ureter and kidney
- An abnormal crossing of blood vessels can press on or distort the UPJ
- Less frequently, UPJ obstructions may form in adults as a result of kidney stones, upper urinary tract infections, surgery, an abnormally crossing blood vessel or swelling in the urinary tract
Treatment:
In many infants with UPJ obstruction, the condition may improve on its own within the first 18 months of life. During this time, repeated ultrasounds and scans are used to monitor the condition to make sure it will not cause lasting harm.
If urine flow doesn’t improve and the obstruction remains after the first 18 months of life, surgery is usually needed to fix the problem [Pyeloplasty]
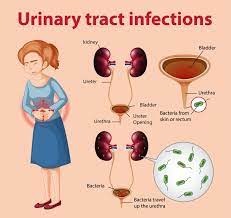 Infection in any part of your urinary system — your kidneys, ureters, bladder and urethra
Infection in any part of your urinary system — your kidneys, ureters, bladder and urethra- Most infections involve the lower urinary tract — the bladder and the urethra
Causes:
- Although the urinary system is designed to keep out microscopic invaders, these defenses sometimes fail. When that happens, bacteria may take hold and grow into a full-blown infection in the urinary tract.
- The most common UTIs occur mainly in women and affect the bladder and urethra
Infection of the bladder (cystitis)
- Escherichia coli (E. coli), a type of bacteria commonly found in the gastrointestinal (GI) tract
- Sexual intercourse may lead to cystitis
- Female anatomy, the short distance from the urethra to the anus and the urethral opening to the bladder
Infection of the urethra (urethritis)
- When bacteria spread from the anus to the urethra
- Sexual intercourse may lead to cystitis
- Sexually transmitted infections, such as herpes, gonorrhea, chlamydia and mycoplasma, can cause urethritis
Symptoms:
- A strong, persistent urge to urinate
- A burning sensation when urinating
- Passing frequent, small amounts of urine
- Urine that appears cloudy
- Urine that appears red, bright pink or cola-colored — a sign of blood in the urine
- Strong-smelling urine
- Pelvic pain, in women — especially in the center of the pelvis and around the area of the pubic bone
Complications:
- Recurrent infections, especially in women who experience two or more UTIs in a six-month period or four or more within a year
- Permanent kidney damage from an acute or chronic kidney infection (pyelonephritis) due to an untreated UTI
- Increased risk in pregnant women of delivering low birth weight or premature infants
- Urethral narrowing (stricture) in men from recurrent urethritis, previously seen with gonococcal urethritis
- Sepsis, a potentially life-threatening complication of an infection, especially if the infection works its way up your urinary tract to your kidneys
Risk factors:
- Female anatomy
- Sexual activity
- Certain types of birth control
- Menopause
- Urinary tract abnormalities
- Blockages in the urinary tract
- A suppressed immune system
- Catheter use
- A recent urinary procedure
Prevention:
- Drink plenty of liquids, especially water Drinking water helps dilute your urine and ensures that you’ll urinate more frequently — allowing bacteria to be flushed from your urinary tract before an infection can begin.
- Drink cranberry juiceAlthough studies are not conclusive that cranberry juice prevents UTIs, it is likely not harmful.
- Wipe from front to backDoing so after urinating and after a bowel movement helps prevent bacteria in the anal region from spreading to the vagina and urethra.
- Empty your bladder soon after intercourse Also, drink a full glass of water to help flush bacteria.
- Avoid potentially irritating feminine productsUsing deodorant sprays or other feminine products, such as douches and powders, in the genital area can irritate the urethra.
- Change your birth control methodDiaphragms, or unlubricated or spermicide-treated condoms, can all contribute to bacterial growth.
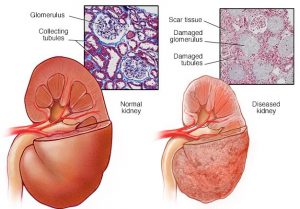 Gradual loss of kidney function
Gradual loss of kidney function- Your kidneys filter wastes and excess fluids from your blood, which are then excreted in your urine. When chronic kidney disease reaches an advanced stage, dangerous levels of fluid, electrolytes and wastes can build up in your body
- Chronic kidney disease can progress to end-stage kidney failure, which is fatal without artificial filtering (dialysis) or a kidney transplant.
Causes:
- Type 1 or type 2 diabetes
- High blood pressure
- Glomerulonephritis, an inflammation of the kidney’s filtering units (glomeruli)
- Interstitial nephritis, an inflammation of the kidney’s tubules and surrounding structures
- Polycystic kidney disease
- Prolonged obstruction of the urinary tract, from conditions such as enlarged prostate, kidney stones and some cancers
- Vesicoureteral reflux, a condition that causes urine to back up into your kidneys
- Recurrent kidney infection, also called pyelonephritis
Symptoms:
- Nausea
- Vomiting
- Loss of appetite
- Fatigue and weakness
- Sleep problems
- Changes in how much you urinate
- Decreased mental sharpness
- Muscle twitches and cramps
- Swelling of feet and ankles
- Persistent itching
- Chest pain, if fluid builds up around the lining of the heart
- Shortness of breath, if fluid builds up in the lungs
- High blood pressure (hypertension) that’s difficult to control
Complications:
- Fluid retention, which could lead to swelling in your arms and legs, high blood pressure, or fluid in your lungs (pulmonary edema)
- A sudden rise in potassium levels in your blood (hyperkalemia), which could impair your heart’s ability to function and may be life-threatening
- Heart and blood vessel (cardiovascular) disease
- Weak bones and an increased risk of bone fractures
- Anemia
- Decreased sex drive, erectile dysfunction or reduced fertility
- Damage to your central nervous system, which can cause difficulty concentrating, personality changes or seizures
- Decreased immune response, which makes you more vulnerable to infection
- Pericarditis, an inflammation of the saclike membrane that envelops your heart (pericardium)
- Pregnancy complications that carry risks for the mother and the developing fetus
- Irreversible damage to your kidneys (end-stage kidney disease), eventually requiring either dialysis or a kidney transplant for survival
Prevention:
- Follow instructions on over-the-counter medications
- Maintain a healthy weight
- Don’t smoke
Benign prostatic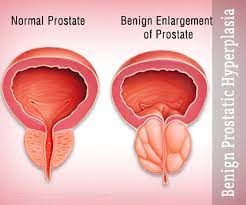 enlargement — also called prostate gland enlargement — is a common condition as men get older.
enlargement — also called prostate gland enlargement — is a common condition as men get older.
Symptoms:
- Frequent or urgent need to urinate
- Increased frequency of urination at night (nocturia)
- Difficulty starting urination
- Weak urine stream or a stream that stops and starts
- Dribbling at the end of urination
- Inability to completely empty the bladder
- Urinary tract infection
- Inability to urinate
- Blood in the urine
The size of your prostate doesn’t necessarily determine the severity of your symptoms. Some men with only slightly enlarged prostates can have significant symptoms, while other men with very enlarged prostates can have only minor urinary symptoms.
Risk factors:
- Aging:About one-third of men experience moderate to severe symptoms by age 60, and about half do so by age 80.
- Family history.
- Diabetes and heart disease.
- Lifestyle: Obesity
Complications:
- Sudden inability to urinate (urinary retention).
- Urinary tract infections (UTIs).
- Bladder stones.
- Bladder damage.
- Kidney damage.
Treatment:
- Medications
Alpha blockers.
5-alpha reductase inhibitors
Combination drug therapy.
Tadalafil
- Transurethral resection of the prostate (TURP)
- Transurethral incision of the prostate (TUIP)
- Transurethral microwave thermotherapy (TUMT).
- Transurethral needle ablation (TUNA)
- Laser therapy
- photoselective vaporization of the prostate (PVP) and holmium laser ablation of the prostate (HoLAP).
- holmium laser enucleation of the prostate (HoLEP)
- Prostatic urethral lift (PUL)
- Embolization
- Open or robot-assisted prostatectomy
- Sympto
 ms related to problems with your lower urinary tract: bladder, prostate and urethra
ms related to problems with your lower urinary tract: bladder, prostate and urethra - LUTS are broadly grouped into symptoms to do with storing or passing urine. You might have symptoms linked mainly to one or the other, or a combination of both.
Symptoms:
- Hesitancy – a longer than usual wait for the stream of urine to begin
- Weak stream
- Straining to urinate
- Dribbling after urination has finished
- A stream that stops and starts
- Feeling an urgent need to urinate
- A short period of time between the urges to urinate
- Waking from sleep to pass urine two or more times a night
- A sudden, intense urge to urinate, followed by urinating without control
Causes:
- Urinary tract infection, or an infection and inflammation of the prostate gland (prostatitis)
- Overactive bladder
- Underlying chronic medical condition, such as obesity, diabetes, high blood pressure, or obstructive sleep apnoea
- Smoking
- Drinking fluids late at night, having too much alcohol or caffeine, or low levels of physical activity
- Difficult to pass urine may be due to enlarged prostate gland, or scarring of your urethra (the tube that carries your urine from the bladder to the tip of the penis
- Some medicines, and diseases such as stroke and Parkinson’s disease
- LUTS is also linked with depression and erectile dysfunction. It’s common to have a number of things that are causing LUTS, so it’s not always easy for doctors to find the exact cause
Prevention:
- Healthy lifestyle and body weight
- Quit smoking
- Treatment of medical conditions such as diabetes, high blood pressure or sleep apnoea
Urethral stri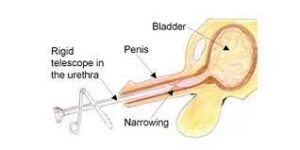 cture is a narrowing of the urethra. Your urethra is the tube that carries urine from the bladder through the penis and out during urination.
cture is a narrowing of the urethra. Your urethra is the tube that carries urine from the bladder through the penis and out during urination.
Causes:
- An injury to your penis or scrotum or a straddle injury to the scrotum or perineum
- An infection, most often sexually transmitted diseases like chlamydia
- Placement of catheters or instruments into the urethra during surgery or procedures
Symptoms:
- Straining to urinate
- Pain during urination
- Urinary tract infection
- Prostatitis
- Retention of urine
Tests:
- Uroflowmetry
- Retrograde urethrogram
- Urinary tract infection
- Cystoscopy
Treatment:
- Urethral dilation
- Internal urethrotomy
- Urethral reconstruction
Visit Us
Zymus Hospital Address
No.1, K NO. 92, Nanjappa Complex, Kanakapura Rd, Raghuvanahalli, Bangalore City Municipal Corporation Layout, Bengaluru, Karnataka 560062
Menu
Quick Links
Copyright © 2024. Dr Anil Kumar T

